General medicine case 6
November 29, 2021
This is an online e-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
A 51 yr old male patient presented to Opd with chief complaints of pedal edema and facial puffiness and fever since 2 months
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 4 yrs back then he developed pedal edema for which he visited hospital and diagnosed as renal dysfunction and he was on medication and dialysis also done once.
In our hospital he was admitted on 31st October 2021 he had complaints of pedal edema since 1 week and shortness of breath since 2 days decreased urine output and was discharged from our hospital on 24th November 2021
But pedal edema not subsided on medication and then they came to our hospital.
And he was put on dialysis thrice a week.
And patient was developing fever from 2 months sometimes before and sometimes after dialysis.
Patient has history of using OTC analgesics frequently for leg pains.
Patient had 10 session of dialysis in our hospital and 2 sessions of dialysis in Hyderabad
DAILY ROUTINE BEFORE ILLNESS:
Patient used to wake up at 5 o clock and he used to climb palm trees for toddy and by 7o'clock patient will return to farm work and he used to eat rice at 10 o'clock in the morning and again returns to farm work and then by 6'o clock in the evening paitent returns to home and complete his natural activities like bathing and take meal at 8 by night and then he goes to sleep.
DAILY ROUTINE AFTER ILLNESS:
Patient wake up at 8 o'clock and the he eats breakfast only one idly and sometimes skips the break fast and then he is not going for any work and complete bed rest now and now he also takes support of his family members for his natural activities like bathing and going to washroom .His apetite was decreased and he is now not having food properly and goes to bed by 8 o'clock at night.
He is known case of hypertension since 2 months and on medication not a known case of diabetes asthma tuberculosis epilepsy.
PERSONAL HISTORY:
Diet :Mixed
Appetite :loss of appetite since 2 months
Bladder movements : decreased urine output since 2 months .
Bowel movements : irregular
Sleep : adequate
Addictions : habit of consuming alcohol since 2yrs
FAMILY HISTORY:
No history of similar complaints in the family
TREATMENT HISTORY:
No history of allergy to known drugs.
GENERAL EXAMINATION:
Patient was concious coherent and coperative well oriented to time place and person.
- pallor present
-No clubbing
-No cyanosis
No icterus
-No generalized lymphedenopathy
-pedal edema present pitting type.
VITALS :
Temperature : febrile
Pulse rate: 90 beats per min
Respiratory rate : 17 cycles per min
Bp :130/ 90mm of Hg..
SYSTEMIC EXAMINATION :
RESPIRATORY SYSTEM
Bilateral airway +
Position of trachea- central
Normal vesicular breath sounds - heard
No added sounds
PER ABDOMEN
Abdomen is soft and non tender
Bowel sounds heard
CENTRAL NERVOUS SYSTEM:
Patient is conscious
Reflexes are normal
Speech is normal.
Blood culture:
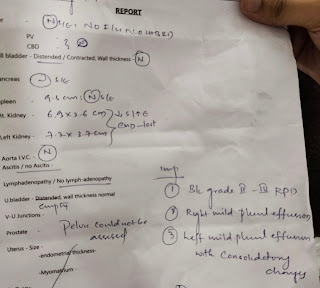
Diagnosis - CKD on MHD
Treatment
Tab lasix 40 mg op /BD
Tab pantop 40 mg po /od
Tab nicardia 10 mg po/TID
Tab orofer po/Bd
Inj iron sucrose 100 mg in NS IV twice
Inj erythropoeitin 400 IV /SC weekly once
Tab nodosis 500 mg po/od
Tab shelchal po/od
Tab vitd3 0.25mg/po/od











Comments
Post a Comment