GENERAL MEDICINE PREFINAL CASE 8
20 December,2021.
INVESTIGATION :
This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardian signed consent. Here we discuss our individual patients problems through a series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
I have been given this case to solve in an attempt to understand the topic of patients clinical data analysis to develop my competency in reading and comprehending clinical data including history, clinical findings, investigation and come up with diagnosis and treatment plan .
A 29 year old male patient supervisor by occupation in Calcutta presented to casualty with the chief complaints of pain in the abdomen since 2 years,radiating to chest and with frequent vomitings and burning sensation since 4 months.
He also complained of pain in his legs since 4
years.
Date of admission : 17/12/2021
HISTORY OF PRESENT ILLNESS :
Patient was apparently asymptomatic 4 months back then he noticed pain in the abdomen which is radiating to chest and with very frequent vomitings and burning sensation in chest region. His episodes of vomiting were 2-3 times per day immediately after having meals.
He has burning micturition and pain while passing stools. He consumes PAN-D tablet immediately after having these symptoms and gets immediate relief.
4 years back in 2016, patient had similar complaints of abdomen pain and vomitings and was diagnosed to have peptic ulcers through endoscopy and was under medication for 6 months .
He also complaints of pain in his calf muscles since 4 years .
Patient complaints of depigmentation of skin with whitish patches over lips.
PAST HISTORY :
K/c/o Renal calculi 4 months back and is under homeopathic medication.
N/k/c/o : asthama, hypertension,diabetes mellitus, epilepsy and tuberculosis.
No previous surgeries.
PERSONAL HISTORY :
Diet : Mixed
Appetite : Loss of Appetite
Sleep : Inadequate
Bowel and Bladder movements : burning micturiton and irregular bowel movements (constipated ).
Addictions : Daily smoker, smokes approximately 10-12 cigarettes or bidis per day since 10 years.
He consumes alcohol occasionally since 10 years.
FAMILY HISTORY :
No similar complaints were there in his family members.
TREATMENT HISTORY :
He is not allergic to any drugs.
GENERAL EXAMINATION :
Patient is conscious, coherant and cooperative.
Clubbing is present.
No pallor,icterus,cyanosis,edema and lymphadenopathy.
VITALS :
BP : 120/80 mmHg
PR: 72bpm
RR: 18 cycles per min
GRBS : 125 mg/dL
SpO2 : 98 %
Temperature : 98.2°F
SYSTEMIC EXAMINATION :
CVS : S1,S2 heard.
No murmurs.
RS : NAB
P/a : soft, non tender.
CNS : No abnormality detected.
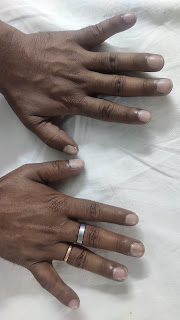
CLINICAL IMAGES :
Clinical image of VITILIGO Problem
Protoscopy cannot be done for anus because of severe pain in the anal region.
PROVISIONAL DIAGNOSIS :
Gastritis with UTI (renal calculi suspecting).
TREATMENT :
Pantop - D 40mg
Zinkomin plus
Pregabalin 75 mg.










Comments
Post a Comment